A UH biomedical engineer is zeroing in on the gap where nerve meets muscle to bring more precise treatment to stroke patients. The National Institutes of Health (NIH) awarded more than $434,000 to Assistant Professor Yingchun Zhang to delve deep into the neuromuscular junction, the connector of the nerve and muscle fiber, to calculate the exact spot to deliver the dose of motion-restoring Botox.
Yes, you read that right: Botox, or Botulinum neurotoxin (BTX), is not just for wrinkles.
The protocol
Botox has long been considered the first-line treatment to reduce spasms in post-stroke survivors, 20-40 percent of whom will suffer continual and crippling muscle spasticity that render them motionless. As a brain disorder, a stroke can cause the brain to send irregular high-frequency signals – through the nerves – to muscles, causing them to keep seizing.
A small gap exists at the neuromuscular junction where “the nerve talks to the muscle,” according to Zhang, by releasing a nano-sized particle called a neuro transmitter. It is inside this gap that Botox must be injected to block the neuro transmitter.
There’s just one problem: No one has ever been able to pinpoint the exact spot of the neuromuscular junction and to confound matters, it varies from patient to patient. To make sure the spot is covered, physicians may use a greater amount of Botox, probably more than necessary – and because Botox has to be repeated every few months, the success rate is not stable.
“Sometimes, even for the same patient with the same physician and same injection protocol – one time it works well, the next time it doesn’t,” said Zhang. He believes he can stabilize the results and reduce the cost of treatment by mapping where the nerve and muscle meet.
Making the map
“We can have an individual map for each patient receiving the injection,” said Zhang. “We can have a 3D map of the gap so the physician will know exactly where the Botox should go. They won’t have to guess or increase the dose.” His 3D model should also be able to reduce the cost of the pricey injections by reducing the necessary dose by about 50 percent.
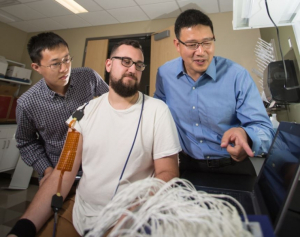
Zhang’s non-invasive approach uses high-density electrodes placed on the surface of the skin. When muscles contract, an electrical discharge is created and he tracks the discharges to the middle point, which is the neuromuscular junction.
“The beauty of this proposal is that we can now go deep into the 3D space of the muscle fiber by using electrical source imaging,” said Zhang.
Bridging the gap
Zhang’s partner in the grant is TIRR Memorial Hermann, widely known as one of the best rehabilitation hospitals in the country.
“We’ll have two groups of patients,” said Zhang. “One will follow the standard approach for the injections and one will use our approach. I think we’re going to beat that group,” he adds excitedly. The victory will come in reducing the costs and side effects while improving the outcome. Zhang’s also excited to see his lab work have a direct and positive effect on people.
The study will continue for two years.
NIH Disclaimer
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health under Award Number R21HD090453. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.