Biomedical engineers at the UH Cullen College of Engineering have identified several new blood biomarkers that can help to predict which lupus patients will progress towards more severe forms of the disease.
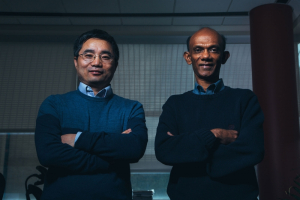
Tianfu Wu, assistant professor of biomedical engineering, and Chandra Mohan, Hugh Roy and Lillie Cranz Cullen endowed professor of biomedical engineering, published their findings last May in the Journal of Proteome Research.
“Our hope is that this research brings the medical field one step closer to screening lupus patients’ blood for biomarkers that can predict which patients are more likely to progress towards renal disease,” Mohan said.
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that affects multiple organs including the kidneys, skin, joints and heart. Roughly 60 percent of all SLE patients experience inflammation of the kidneys, called lupus nephritis. Kidney disease is a leading cause of death among SLE patients – roughly a quarter of all lupus patients succumb to end-stage renal disease.
Early detection and management of lupus nephritis can significantly increase a patient’s quality of life and chances of survival. Currently, clinicians have no way to predict which lupus patients will progress towards kidney disease.
Renal biopsies – a procedure in which the kidney is punctured and a tissue sample is extracted for further analysis – are the gold standard for diagnosing kidney disease. However, the procedure is invasive and can’t be repeated serially because of potential complications.
“There is an urgent need to identify biomarkers for lupus nephritis that enable early detection, intervention and follow-up of the disease,” Mohan said.
To identify new biomarkers for the disease, Mohan and Wu studied blood samples collected from 22 SLE patients and 22 healthy controls using antibody-coated glass slide assays, a novel technique for analyzing proteins in human blood samples. The glass slide assays allowed the researchers to analyze 274 proteins in the blood at once, where standard assays could only analyze a handful of proteins at a time.
“This is one of the largest screens ever conducted for lupus in one single shot,” Mohan said.
Results from the screening showed 48 possible proteins that were elevated in the lupus patients’ blood.
To validate these findings, the researchers used an ELISA assay – a well-accepted biochemical technique for detecting the presence of molecules in a sample – to study the blood samples of an independent cohort of 28 SLE patients and 28 healthy controls.
Results from the ELISA assays revealed the top 12 proteins that were elevated in the blood of lupus patients compared to healthy patients. Furthermore, the researchers identified several proteins that were elevated in patients’ blood with active lupus nephritis.
Lupus is a puzzling disease, characterized by disease flares and remissions. During an active state of the disease – also known as a flare – the body’s immune system begins attacking its own organs and tissues, and a patient’s renal function can deteriorate.
“We found that levels of several molecules are increased, especially in patients with active kidney disease, suggesting that these proteins could potentially be markers for identifying patients that will go into disease flares or kidney function deterioration,” Mohan said.
Mohan and Wu further validated these results by collecting blood samples from another independent cohort of 45 patients with active lupus nephritis at the time they were undergoing a kidney biopsy. The idea behind this phase of the study was to “correlate the levels of the proteins found in the patients’ blood with exactly what was going on in their kidneys at that time,” Mohan said.
After a renal biopsy is conducted, the physician assigns two important scores to quantify kidney function: a chronicity index and an activity index. Mohan and Wu found that elevated levels of three blood proteins in particular were correlated with impaired kidney function scores on the chronicity index, activity index or both.
“This means we have hope to try to predict what’s happening in the kidney simply by measuring these three proteins in the blood, which would allow patients to avoid invasive renal biopsies,” Mohan said.
Finally, the researchers tracked seven lupus patients over the course of one year, collecting their blood samples at three consecutive check-ups with their physicians. The goal of the final phase of the study was to monitor the potential blood biomarkers over time to see if the severity and activity of each patient’s disease correlated with elevated levels of the identified proteins in the patients’ blood samples.
Mohan and Wu discovered several proteins that correlated with the patients’ disease activity over time to different degrees. However, no single marker was connected to lupus activity in all of the patients or in all of the screenings conducted.
These findings are consistent with what researchers have managed to learn so far about the complex and mysterious disease, which has been shown to present differently from patient to patient.
“We see lots of variability between lupus patients,” Mohan said, adding that identifying more markers for the disease could lead to greater understanding of its causes. “One take home message here is that we can possibly begin to subset lupus patients based on what blood biomarkers they express.”
The researchers will be expanding their research to analyze more than 1,000 biomarkers for lupus, both in the blood and the urine, hoping to identify patterns of biomarkers that can be used to subset the many different types of lupus patients.
Although further validation through longitudinal clinical studies involving many more lupus patients is required, Mohan and Wu agree their research is a very important step towards predicting health outcomes for lupus patients.
This research was supported by grants from the National Institutes of Health (NIH) and the Lupus Research Institute.