Sergey Shevkoplyas wants to make one thing perfectly clear: Blood transfusions save millions of lives every year. Without them, routine surgeries would become life threatening. They’re one of modern medicine’s absolute necessities.
But that doesn’t mean transfusions are perfect. There’s strong evidence that for some patients, transfusions of red blood cells stored in a refrigerator for prolonged periods of time can be dangerous or even deadly.
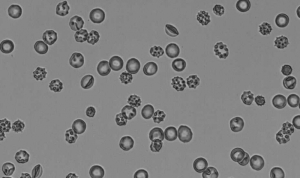
That’s because patients get more than just healthy, well-preserved red blood cells during a transfusion. They also get a number of materials that are potentially harmful, including the anticoagulant-preservative solution that keeps red blood cells alive throughout storage; cells that have been irreparably damaged by processing the blood after donation and during storage; the remnants of burst cells, including free hemoglobin and microparticles that can contribute to inflammation and the formation of blood clots; and the byproducts of cellular metabolism (essentially cellular waste). The longer blood is in storage, the more these materials build up.
“Therapeutically, there’s absolutely no reason to transfer any of this into the patient,” said Shevkoplyas, associate professor of biomedical engineering with the University of Houston Cullen College of Engineering. “The only thing you need to transfuse into the patient are well-preserved red blood cells. There’s no point to giving you these other potentially toxic materials.”
The National Institutes of Health clearly agrees, and has given Shevkoplyas an NIH Director’s Transformative Research Award to develop a simple device to separate healthy, well-preserved red blood cells from all the other material in the blood bag just before transfusion. Such grants support high-risk/high-reward projects with potentially transformative impacts. The $1.8 million award was originally given in 2012 while Shevkoplyas was at Tulane University and the remaining $1.5 million was recently transferred to UH.
The system Shevkoplyas is developing will consist of two tubes that feed into a plastic device just a few inches in size. One tube will send blood into the device while another will send saline solution. In the first step, the saline will literally wash harmful particles and the storage solution off the healthy red blood cells.
Next, the entire mixture will be sent through an array of precisely designed microfluidic channels. There the shape, size and flexibility of healthy red blood cells will allow them to be separated from the particles, damaged cells, and storage solution. At that point, the healthy red blood cells, along with saline acting as a transport medium, can be safely transfused into the patient.
None of this will be easy, said Shevkoplyas. Most microfluidic research (where fluids flow through channels measuring less than a millimeter) involves devices that can handle just a few drops per hour. With its series of interconnected channels, Shevkoplyas’ device aims to scale these microfluidic interactions “up by a factor of 1,000.”
“That’s the big challenge. Adapting our understanding of microfluidics to a high-throughput device turns out to be not very simple, though we do have some good data to show we can do it,” he said.
While Shevkoplyas’ system faces significant scientific and engineering hurdles, one of its biggest advantages is just how practical it is.
The materials Shevkoplyas will use to build the device, like the saline solution, are already approved by the U.S. Food and Drug Administration. This significantly reduces the burden for regulatory approvals, which should help keep the cost of the system at around $50 and allow it to come to market sooner.
In addition, since healthcare systems worldwide have invested billions of dollars into existing blood storage and transfusion practices, using the device won’t require any significant changes to these practices. Instead, the small, disposable device would be placed between the blood bag and the patient during transfusion, completely at the discretion of the patient’s care team.
Together, these features make it much more likely that Shevkoplyas’ device will move from the lab to clinical use, where it can have a positive impact on patient health.
“We’re trying to fit as much of this device as we can into the existing paradigm of transfusion. We want to empower medical professionals at the scene to make the decision about using this system,” said Shevkoplyas. “You cannot save people’s live without blood transfusions. We’re just trying to make this life-saving procedure as safe as possible.”