A researcher with the University of Houston Cullen College of Engineering has won a grant to make brain surgery for patients with severe cases of Parkinson’s disease safer and more effective.
The grant goes to Nuri Ince, an assistant professor of biomedical engineering. Awarded by the National Science Foundation, it is valued at $330,000 for three years of work.
Ince, in collaboration with Aviva Abosch, an M.D./Ph.D a neurosurgeon with the University of Colorado School of Medicine, will use the funds to improve deep brain stimulation (DBS) surgery.
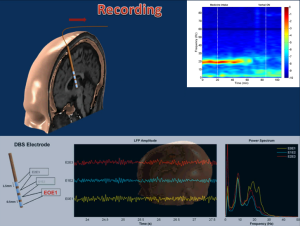
In this surgery, an electrode measuring just a few millimeters across is inserted into the brain. When attached to a small battery pack, a series of contacts on the electrode can be used to both stimulate and record electrical activity in nearby neurons.
The target of the probe is the subthalamic nucleus (STN), a small, football-shaped section of the brain that helps control movement. In Parkinson’s patients, the STN is misfiring, causing symptoms like tremors and labored movement. For most patients, these symptoms can be managed by medication. Some, though, don’t respond to medicine. If their symptoms become severe enough, they may opt for DBS surgery.
One of the major challenges in DBS surgery is getting the electrode to just the right spot. The STN sits nearly 3 inches below the scalp and is very tiny – just 6 millimeters by 4 millimeters. This makes hitting the STN with the probe extremely difficult, Ince said. And that’s the exact problem he aims to solve.
Currently, surgeons insert several microelectrodes into the brain in order to record electrical activity that hopefully will reveal the STN’s location. It is very difficult, though, for neurosurgeons to interpret this activity, especially during an actual surgery.
It also neglects the abilities of the probe that targets the STN, Ince said. The contacts on this probe can not only stimulate electrical activity, but also record it. Ince, then, is developing signal-processing techniques that interpret the electrical activity recorded by the probe. These techniques will provide feedback to neurosurgeons about the location of the STN in real-time, allowing them to guide the placement of the probe accordingly. This will allow an entire DBS surgery to be performed faster and more accurately than ever before.
“We first record the electrical activity of the brain, and then by doing signal processing, we are trying to understand if we’re at the right location and which contacts should we use,” he said. “The activity we record from the contacts actually gives us clues.”
This is especially important given the facts of DBS surgery. Patients must stay awake through the entire procedure in order to show how they’re responding to electrical stimulation. Whether their tremors decrease or not, for instance, can provide important information to the surgical team. Since staying awake during brain surgery can be traumatic, technologies that can shorten surgical time are valuable.
In addition, the technology can eliminate the need to insert the probe multiple times in order to find the STN. Fewer insertions mean less bleeding, shorter surgeries and faster recovery times, Ince said.
To conduct this work, Ince will be present during deep brain stimulation surgeries, during which he will attempt some data interpretation and provide doctors with real-time guidance on probe placement.
He will then take information recorded during these procedures and attempt to build signal-processing technologies that can automatically provide this direction. “We want to give intelligent feedback to the surgeon. If the neurosurgeon can get some clues, that’s very useful. It should result in more effective surgeries and better patient outcomes,” he said.