A researcher with the University of Houston Cullen College of Engineering has won a grant to develop new treatments for the most deadly form of pediatric brain cancer.
Navin Varadarajan, assistant professor of chemical and biomolecular engineering, and Laurence Cooper, an M.D./Ph.D. with The University of Texas M.D. Anderson Cancer Center, won the two-year, $250,000 grant from Alex’s Lemonade Stand Foundation. This is the latest in a series of grants the pair has won. In 2012 they received a combined $3.4 million from the National Institutes of Health and the Cancer Prevention and Research Institute of Texas to conduct two separate studies targeting leukemias and lymphomas.
The subject of this latest award is diffuse intrinsic pontine glioma, or DIPG, a type of brain cancer that typically strikes children before their 10th birthday.
The disease appears at or near the brain’s connection to the spinal column. This location, combined with the tumor’s tendency to grow among nerves that are responsible for everything from movement to breathing, make it impossible to treat DIPG with surgery. Other therapies have proven largely ineffective, as well. As a result, the disease is considered universally fatal, with most patients dying within a year of their diagnosis.
Since more established therapies don’t work on DIPG, Varadarajan and Cooper are exploring treatments based on one of the newest methods for fighting cancer: immunotherapy.
In immunotherapy, human immune system cells are modified to fight a specific disease. This project focuses on engineered T-cells, immune cells that, among other functions, recognize and attack disease cells.
The researchers are modifying naturally occurring T-cells to recognize and attack DIPG cells. Known as chimeric antigen receptor T-cells, or CAR T-cells for short, these modified cells have proven effective in combating cancers that are particularly difficult to treat.
"In response to tumor recognition, CAR T-cells can proliferate within the patient. Unlike traditional drugs that are removed from the body, these cells can multiply. The better these CAR T-cells proliferate and survive within the host, the better the chances of getting rid of the tumor," said Varadarajan.
The ability of CAR T-cells to proliferate, though, can also be one of the biggest challenges to immunotherapy, Varadarajan added. If CAR T-cells are too active, they can actually trigger an overly aggressive immune response that ends up killing healthy cells. Given that DIPG tumors reside in the brain, such a response could be devastating.
The researchers, then, must develop DIPG-fighting CAR T-cells that trigger an immune response strong enough to fight the cancer but then shut off before damaging healthy cells.
While Cooper will modify the naturally occurring T-cells to respond to DIPG, this effort faces one of the biggest challenges in all of biomedical research: how to study these individual cells. Typically, researchers are limited to studying large populations of cells, making it difficult to extensively characterize them and to note subtle but important differences.
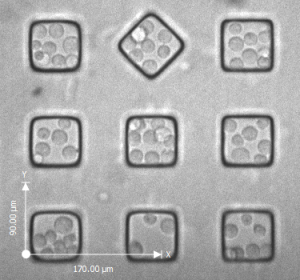
Solving this problem is where Varadarajan’s expertise lies. He has created a special slide, dubbed the nanowell array, capable of isolating individual cells. The array has tens of thousands of chambers carved into a few square centimeters. Each of these chambers measures about 125 picoliters in volume – just the right size to capture one or two individual cells.
Varadarajan and his collaborators, then, will expose populations of CAR T-cells DIPG cancer cells to the nanowell array. They will then study how the engineered CAR T-cells react to the cancer.
Their findings will allow them to select the most promising strains of CAR T-cells for further research and modification, first using petri dishes, then animal models. In the longer term, they plan to apply this work to clinical trails of DIPG patients.
“Immunotherapy is at the forefront of cancer treatment and research. In some cases it has actually resulted in complete remission," Varadarajan said. "To help the most people, though, we’ve got to understand exactly what properties of engineered cells are most effective at fighting cancer. This research will help us quickly identify those properties so they can be included in the future rounds of research and clinical trials.”